Explore our range of payroll and HR solutions built for companies with 50–999 employees.

It’s time to get the HR and payroll solutions you need to help you:
Align
Your challenges are as unique as your business — meaning a one-size-fits-all HR solution just won’t cut it. We work with you to align your people and financial strategies by diagnosing your exact needs and offering a range of tailored solutions. Our all-in-one HR suite, including flexible service models, such as outsourcing and PEO, as well as pre-integrated solutions from ADP Marketplace, save you time and money, allowing your business to do more.

Whatever your HR or payroll challenge, we’ve got you covered.
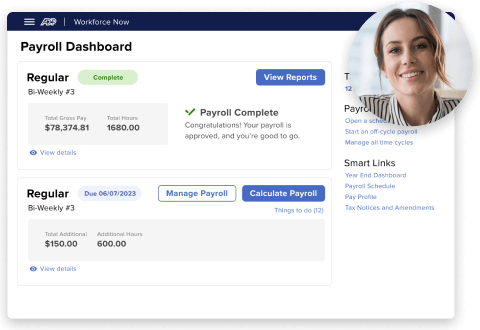
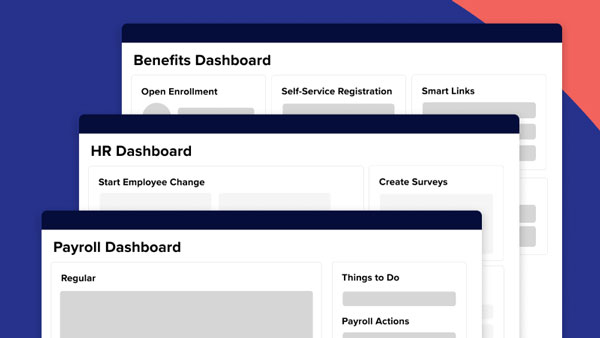
Work and pay your way with our all-in-one HR suite that handles everything from hire to retire:
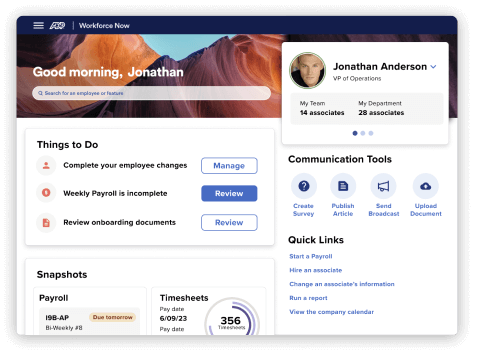
A premium partnership backed by deep HR expertise — get what you need to deliver powerful results at any scale for your HR, payroll, talent and benefits administration needs.
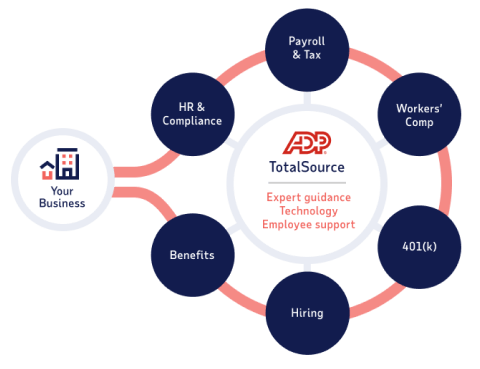
ADP TotalSource is the nation’s largest all-in-one, full-service PEO solution:
Our packages are designed to meet any HR and payroll needs — and to provide more value to
your organization by helping your team thrive.
Plus
Everything included in our "Select" package and streamline benefits administration with time-saving technology.
Premium
Everything included in our "Plus" package and automated time-tracking with Time and Attendance.
Optimize
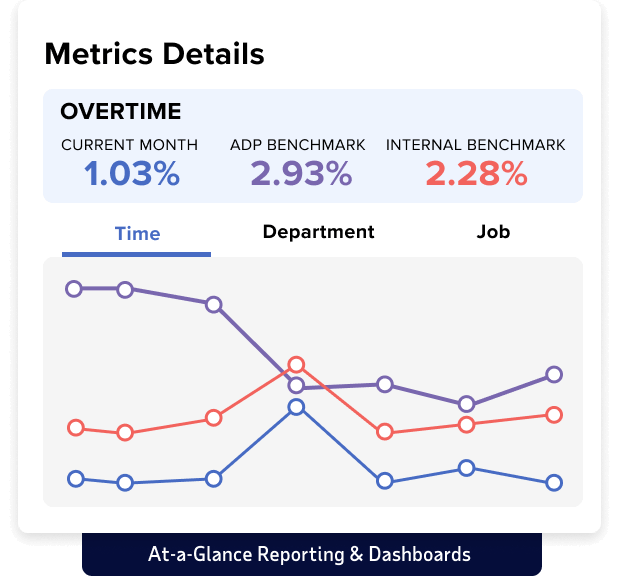
With ADP, you gain access to the world’s largest HCM benchmarking data set. This gives you the power to analyze current market trends and make proactive, data-driven decisions around salary compensation benchmarking, DE&I insights, benefits enrollment and much more.
See for yourself how it works or schedule a demo for a deeper dive.
1-minute video
See how our single, scalable HR suite is designed to help your workforce thrive.
Protect
Peace of mind can be hard to find in times of growing cybersecurity and economic threats. But throughout our history, we’ve proven time and time again our ability to protect businesses from risk — all while instilling confidence and continuity through times of uncertainty. This is what you get with the world’s largest and most trusted HR and payroll provider.
MEET OUR CLIENTS
If you're looking for a company that is going to provide you with excellent service, capabilities and efficiency, then the only option you have is ADP.
Pia Saks Payroll Manager, Vanderbilt Global Services

MEET OUR CLIENTS
ADP has done a great job of integrating the functions of its various products into one operating system.
Tony Harmon Payroll/HR/Benefits Administrator, MACK II, Inc.

MEET OUR CLIENTS
The ADP Compensation Management module is, by far, the biggest time saver that we have implemented. Our previous process literally took weeks to roll out and complete. Now, we can accomplish it in about day. That is so much time saved. The compensation module has been a life changer.
Watch Testimonial See case study
Theresa Allen Payroll Specialist/HR administrator, Home Federal Savings Bank


analyst report
guidebook

case study

Your privacy is assured.
