Questions about W-2s or 1095-Cs? Get guidance here:
For Employees: W-2 & 1099 • 1095-CFor Employers: W-2 & 1099 • 1095-C
Answer a few questions, and we'll help you find the perfect HR and payroll solution.
You need comprehensive payroll and HR solutions that empower your people and unlock your teams’ potential. We deliver.
Select your business size to try a demo today. Select your business size to
try a demo today.
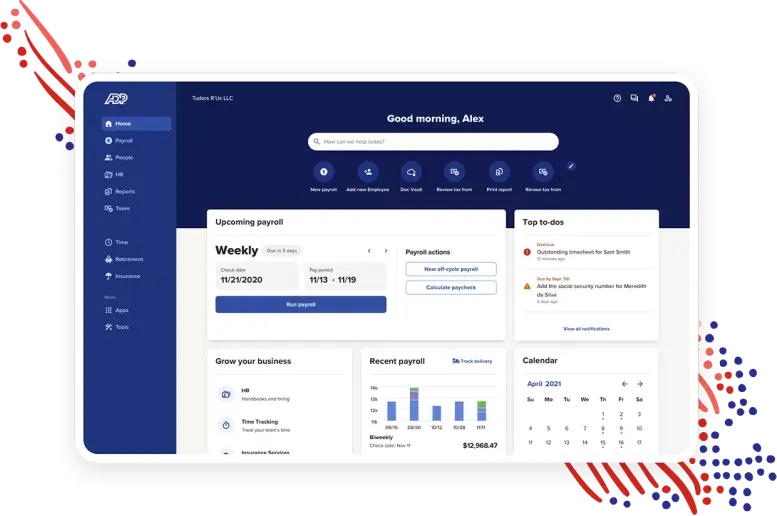

1-49 Employees
Faster, easier, more reliable solutions designed to help you focus on what matters.

50-999 Employees
Superior HR tech and services designed to help you manage your entire workforce with ease.

1000+ Employees
Adaptable HCM designed to drive people performance and keep ahead of continual change.

MEET THE TEAM


17 consecutive years


2023

2022

8 consecutive years

11 consecutive years
* From Fortune. ©2023 Fortune Media IP Limited All rights reserved. Used under license. Fortune® is a registered trademark and Fortune World’s Most Admired Companies™ is a trademark of Fortune Media IP Limited and are used under license. Fortune and Fortune Media IP Limited are not affiliated with, and do not endorse products or services of, ADP, Inc.
Any time you select a partner, you're looking for 2 things: great technology and a great team to work with. With ADP we have both. Our ADP team is knowledgeable and there to advise us and answer our questions. That, combined with ADP's robust and adaptable global technology gives us confidence that our employees are taken care of.
Greg Harmer
Global Head of Payroll, Amazon
![]()


Discover the full body of new Today at Work insights from the ADP Research Institute
How to measure the performance and impact of HR through the lens of the employee experience
Your privacy is assured.